Surbex Z tablets Detail 2024 , Surbex Z tablets Benefits and side effects 2024
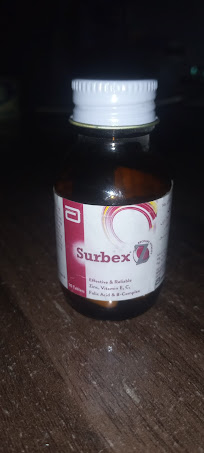
Surbex-Z is a multivitamin and mineral supplement that is often used to help address nutritional deficiencies and support overall health. It contains a combination of vitamins and minerals that can offer several potential benefits when taken as part of a balanced diet and a healthy lifestyle. Here are some of the potential benefits of Surbex-Z tablets: As of my last knowledge update in January 2022, Surbex Z is a multivitamin supplement. It typically contains a combination of vitamins and minerals, such as vitamin C, vitamin E, zinc, and selenium. These nutrients play various roles in the body, including supporting the immune system, promoting healthy skin, and participating in various metabolic processes. It's important to note that specific formulations of multivitamin supplements can vary, and new products may have been introduced since my last update. Additionally, recommendations for vitamin and mineral supplementation should ideally be discussed with a healthcare profess...



Comments
Post a Comment
If you have any doubts Please let me now